Claims Analysis & Data Analytics Services
Underwriting Services
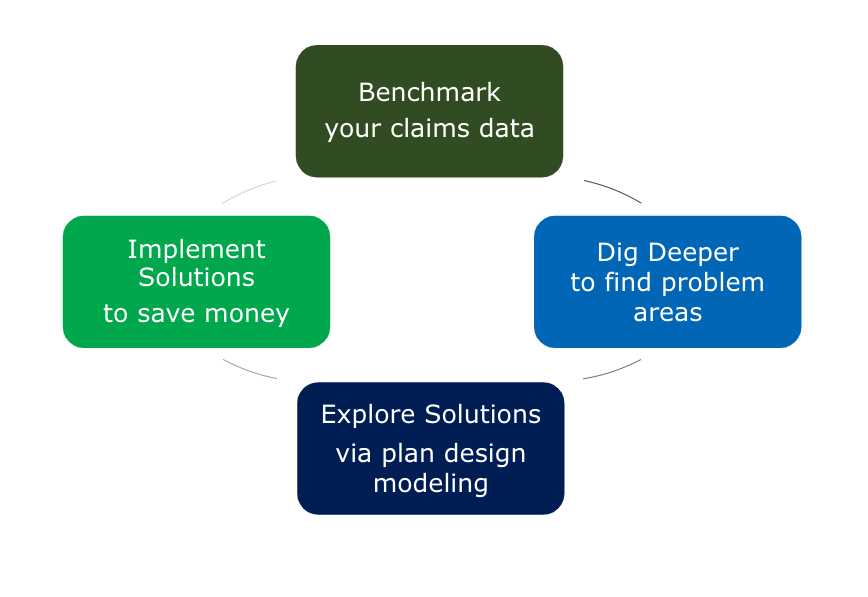
MDG’s in-house underwriting department provides comprehensive claims analysis as well as vendor audits. Agency underwriters analyze monthly claims and diagnosis reports to identify key drivers of cost. The data are sorted into an actionable format and utilized to inform the employer’s benefit strategy in terms of plan design changes, wellness program initiatives, funding arrangements, stop loss management, and pharmacy benefit management contracting.
Claims frequency analysis compares the employer’s utilization to book of business norm to identify cost outliers. High-cost claims diagnosis information is evaluated to inform future stop loss limit decisions to assure proper financial protection and risk management. We evaluate pharmacy rebate revenue received to continually assure our clients’ provider contracts maximize available savings.
MDG’s underwriting department provide the following services:
- Alternative Funding Strategy
- Benefit plan change modeling
- Employee premium share modeling
- IBNR Reserve Calculation
- Budget strategy support
- Health Care Reform cost impact modeling
- Employer specific trend analysis and forecasting
- Retention fee analysis
- Demographic monitoring & analysis
- Customized monthly claims reporting & summaries
- Network provider pricing comparisons
- Renewal projections
- Disease management evaluation and ROI
- Wellness program ROI